This is a hypothetical patient case developed for educational purposes by Henry Nasrallah, MD, based on characteristics of patients with tardive dyskinesia as seen in clinical practice. The hypothetical case was sponsored and co-developed by Neurocrine Biosciences.
Ava J. is a 50-year-old divorced mother of 3 with a history of bipolar disorder. She was referred by a community psychiatrist for abnormal facial movements not responding to benztropine.
She appears somewhat depressed and anxious—she reports no mania or hypomania symptoms since her last visit 4 months ago, but she is distressed by worsening mouth movements and involuntary grimacing.
Patient Information
- Name: Ava J.
- Age: 50 y
- Sex: Female
- Race/Ethnicity: African American
- BMI: 26
- BP: 160/100 mm Hg
- Current problems:
- Bipolar disorder
- Abnormal facial movements
- Diabetes
- Hyperlipidemia
- Hypertension
- Current medications:
- Risperidone 2 mg BID
- Benztropine 1 mg BID
- Lamotrigine 200 mg daily
- Metformin 1000 mg daily
- Verapamil 180 mg daily
BID, twice daily; BMI, body mass index; BP, blood pressure.
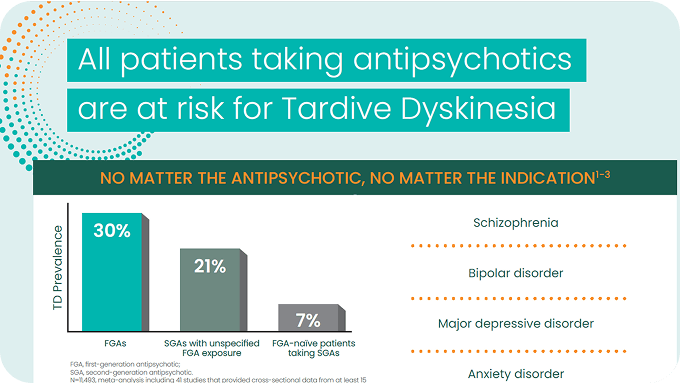
Ava was diagnosed with bipolar disorder in her early 30s and was treated with a first-generation antipsychotic and lithium for about 8 years. Ten years ago, this medication regimen was changed to a second-generation antipsychotic and lamotrigine, which she has been relatively stable on for the past 10 years.
Psychiatric History
- Current diagnosis: Bipolar disorder
- Previous psychiatric diagnoses: None reported
- Current psychiatric medication: Risperidone 2 mg BID, lamotrigine 200 mg daily
- Psychiatric medication history: Haloperidol 15 mg daily, lithium 300 mg TID (both stopped 10 years ago)
- Safety concerns: None reported
- Previous psychiatric hospitalizations: 4 hospitalizations for bipolar disorder
- Substance use: None reported
TID, 3 times daily.
Early on in the course of her bipolar disorder, Ava experienced oculogyric dystonia following haloperidol IM. She also has a history of akathisia and drug-induced parkinsonism and has been taking benztropine for 4 years. Recently, her facial movements have been getting worse and she is anxious because she cannot control them. She says that lip and tongue movements interfere with chewing and she has given up trying to wear lipstick. She thinks the movements are related to her medication regimen, but doesn’t understand why they are getting worse, because benztropine “is supposed to help them.”
History of Movement Disorders
- History of oculogyric dystonia after haloperidol IM
- History of akathisia and drug-induced parkinsonism
- Treatment with benztropine 1 mg daily for 4 years
IM, intramuscular.
The psychiatrist and resident conducted a thorough motor examination, AIMS exam,1 and history. Abnormal facial and oral movements that were irregular in rhythm were documented, including lip pursing, tongue darting, and eye grimacing. Her AIMS total score was 7.1 These observations, combined with her history and chronic treatment with antipsychotics,2 led to a diagnosis of TD.
Motor Evaluation
- Abnormal facial and oral movements
- Lip pursing, tongue pushing against teeth and darting in and out, eye grimacing
- Absence of cogwheeling, truncal rigidity, or shuffling gait; arm swing is normal
- History of several years’ exposure to haloperidol and risperidone–consistent with TD
- AIMS total score: 7
AIMS, Abnormal Involuntary Movement Scale.
The psychiatrist provided Ava with education about TD and the available treatment options. Ava expressed that the movements are causing her emotional distress and that she wanted to try treatment with a VMAT2 inhibitor. The psychiatrist initiated treatment of her TD with a VMAT2 inhibitor and scheduled a follow-up appointment in 1 month.
Notes From Today's Visit
- Patient provided with education on TD and the risk for additional symptoms
- Began treatment with a VMAT2 inhibitor
- Scheduled a follow-up appointment in 1 month
References
1. Rush JA. Handbook of Psychiatric Measures. 2000:166-168.
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
©2022 Neurocrine Biosciences, Inc. All Rights Reserved.
MED-MSL-TD-US-0222 v2 CP-TD-US-0678 v3 10/2022